- Home /
- Conditions /
- Back Pain /
Find Relief with Back Pain Treatment in NJ
Back pain can be caused by a wide range of issues from disc herniations to sciatica. Find out more about conditions, causes and common treatment options for back issues.


Back Pain: Conditions, Causes and Common Treatment Options
Back pain is a common problem, with as many as 80% of people experiencing it at some point in their lives. The reasons for back pain can range from minor issues like a sprained muscle to more severe issues such as degenerative disc disease or slipped discs.
The treatments for back pain can vary as widely as the reasons for it. In some cases, rest and over-the-counter medications can address an issue, however most will require some form of treatment to restore normal function. In some cases, surgery may be required. Between those extremes are a plethora of natural, traditional and alternative treatment options for back pain.
Find out more about common back problems, their impact on the body and potential treatments below.
Treatments for Back Pain
 Epidural Injection
Epidural Injection
 Facet Block
Facet Block
 Medial Branch Block
Medial Branch Block
 Radiofrequency Ablation
Radiofrequency Ablation
 Sacroiliac Joint Injection
Sacroiliac Joint Injection
 Spinal manipulation
Spinal manipulation
 Spinal Decompression
Spinal Decompression
 Spinal Traction
Spinal Traction
 Exercise Rehab
Exercise Rehab
 Sport Specific Rehab
Sport Specific Rehab
 Needle acupuncture
Needle acupuncture
 Cupping
Cupping
 Gua sha
Gua sha
 TENS and EMS
TENS and EMS
 MLS Laser Therapy
MLS Laser Therapy
 Kinesio Tape
Kinesio Tape
 Graston Technique
Graston Technique
 Active Release Technique (ART) for Soft Tissue Injuries
Active Release Technique (ART) for Soft Tissue Injuries
 mild® Procedure in NJ
mild® Procedure in NJ

Disc Herniations

What Are Disc Herniations?
The spine is made up of 24 bones called vertebrae, which are supported by round discs, ligaments and muscles. Between each of these bones or vertebrae is a soft gelatinous disc that has an inner core called a nucleus and an outer layer called the annulus. Disc herniation occurs when the annulus of a disc ruptures or tears, allowing the nucleus to be pushed into the spinal canal.
The symptoms of disc herniation vary based on where the herniation occurs and how severe it is. A small herniation that doesn’t press on a nerve may cause no symptoms at all, or it may cause a dull ache in the lower back. If the disc herniation presses on a nerve, the condition may cause radiculopathy, a group of symptoms that includes pain, numbness, tingling and weakness. Herniations in the neck, also known as the cervical spine, may cause neck pain, pain between the shoulder blades and pain that radiates from the neck to the arm or headaches.
How Common Are Disc Herniations?
Each year, disc herniations affect millions of people. It is estimated that five to 20 out of every 1,000 adults, with approximately 1 to 3% of herniations causing symptoms. Disc herniation is more common in men than women, and it usually occurs between the ages of 30 and 60.
Common Treatments for Disc Herniations
Nonsteroidal anti-inflammatory drugs (NSAIDs) chiropractic care and physical therapy are usually the first treatments used to address the symptoms of disc herniation. If conservative treatment doesn’t work epidural steroid injections or surgery can help relieve the symptoms.
A surgeon may be able to remove the herniated disc, preventing the disc fragment from pinching nerves in the spinal canal. Some surgeons recommend spinal fusion as a treatment for disc herniation. During this procedure, two of the vertebrae are fused together. The procedure makes the spine more stable and relieves the symptoms of disc herniation.
Sciatica

What Is Sciatica?
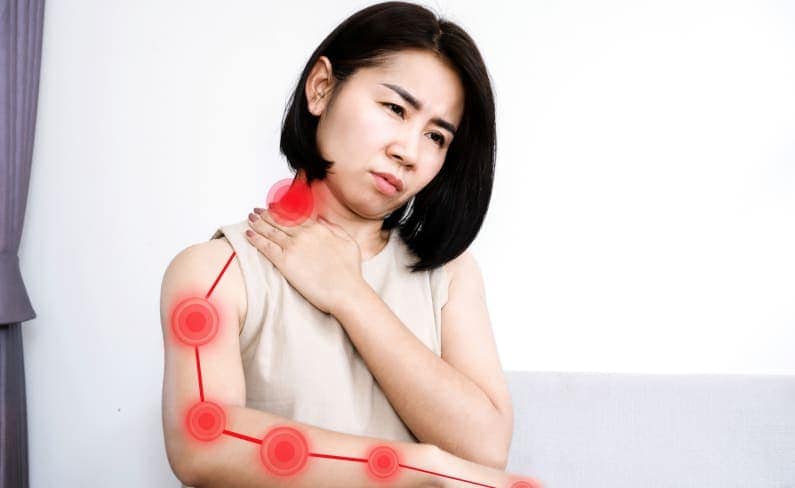
Sciatica is pain that radiates from the lower back through the buttocks and down the leg on one side of the body. Caused by injury to or pinching, compression, inflammation or irritation of the sciatic nerve, the pain may be mild to severe and may feel like a shooting jolt of pain. The pain may remain constant, or it may be intermittent. Turning the body, making sudden movements, coughing or sneezing may cause sciatica pain to occur if you’re dealing with this condition. Other symptoms can include numbness and muscle weakness in the affected leg.
How Common Is Sciatica?
Back pain is the third-most-common reason people seek medical care, and approximately 40% of Americans experience sciatica at some point in their lives.
Age-related changes in the spine, such as bone spurs and herniated discs, often lead to compression of the sciatic nerve. People who are obese, have diabetes, sit for long periods or engage in physically rigorous activities or occupations are prone to developing sciatica.
Common Treatments for Sciatica
Sciatica symptoms may resolve within four to six weeks, and sometimes no treatment is necessary. Applying hot or cold packs and taking over-the-counter pain medications, such as nonsteroidal anti-inflammatory drugs, may help alleviate discomfort. Gentle stretches may also be helpful.
If self-help measures don’t provide relief within six weeks, a physician may prescribe stronger pain relievers or muscle relaxers. Spinal injections and physical therapy may also alleviate pain. Surgery may be an option if other treatments fail to provide relief within 12 months or if loss of bowel or bladder control occurs.
Some people find alternative therapies helpful in treating sciatica. Chiropractic, massage therapy, acupuncture and yoga may provide relief. Some individuals also find that biofeedback aids in pain and stress management.
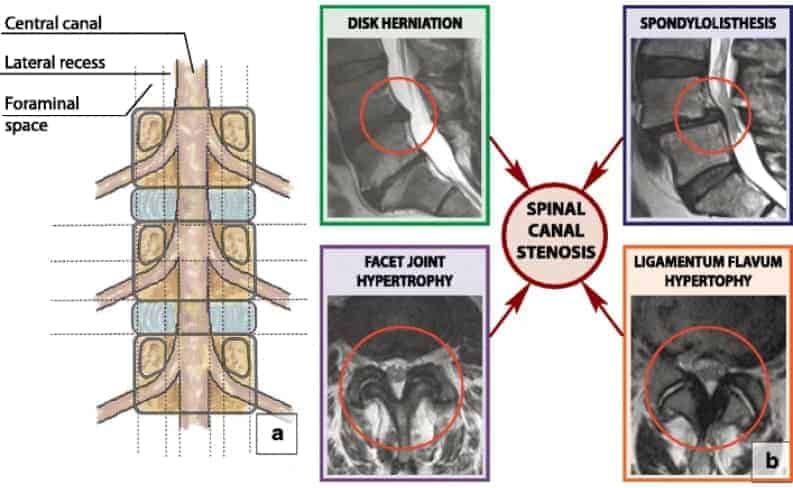
Stenosis
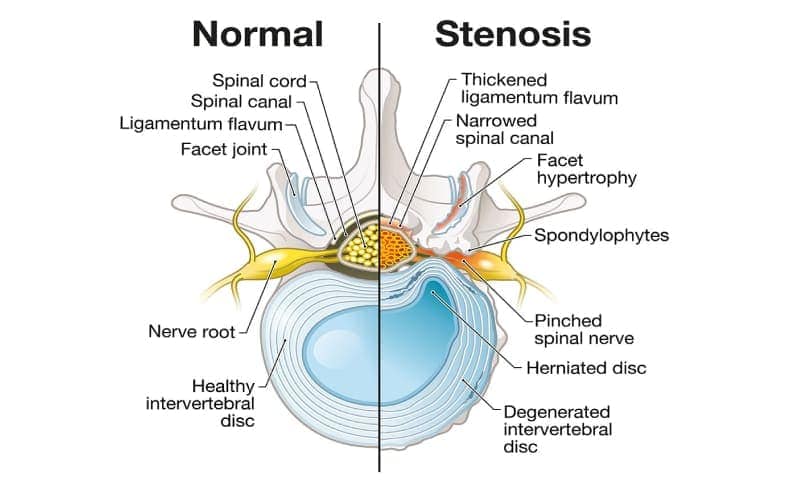
What Is Stenosis?
Stenosis is the narrowing of one or more spaces in the spine. As the narrowing progresses, the nerves and spinal cord may become compressed, pinched or irritated. Because this narrowing usually takes place gradually, symptoms may not be present initially, but pain may develop over time.
Stenosis can occur in any part of the spinal column, but it most often is seen in the neck (cervical region) and in the lower back (lumbar region). A person with cervical spinal stenosis may have neck pain, numbness and/or weakness in the hands and arms and problems with balance.
Lumbar Spinal Stenosis (LSS)
Lumbar spinal stenosis (LSS) is a medical condition characterized by the narrowing of the spinal canal in the lower back. This narrowing can compress the nerves within the spine, leading to various symptoms such as lower back pain, numbness or weakness in the legs, and difficulty with walking. In rare cases, loss of bowel and bladder control may occur. LSS often develops gradually, primarily affecting older adults, and can significantly impact an individual’s daily life and mobility.
How Common Is Stenosis?
Although some people are born with spinal stenosis or receive an injury that leads to the condition, it can be caused by gradual, age-related changes in the spine. As many as 95% of people develop degenerative spinal changes by their 50th birthday, and spinal stenosis primarily occurs in those over age 60. Spinal stenosis affects both men and women.
Common Treatments for Stenosis
Some people find relief from symptoms by applying hot or cold packs to the affected area. Specific exercises that strengthen back muscles and improve balance and flexibility may also help. Physical therapy, chiropractic adjustments and acupuncture alleviate pain in some cases. Over-the-counter and prescription pain relievers and muscle relaxers may be beneficial as well.
More invasive treatments include steroid injections to help reduce inflammation. If other treatments fail to produce desired results, several surgical procedures are available to remove thickened ligaments, bone, bony growths or disks or to fuse two vertebrae.
mild® Procedure
The mild® procedure is an advanced, minimally invasive treatment designed for individuals dealing with lumbar spinal stenosis (LSS). It effectively alleviates LSS symptoms by gently removing excess ligament and bone tissue, creating more space within the spinal canal. This results in pain reduction and improved mobility, with a faster recovery and minimal postoperative discomfort, making it a preferred option for those seeking relief from LSS.
Spondylosis
What Is Spondylosis?
Spondylosis refers to the changes that occur to the ligaments, cartilage, bones and discs in the spine as a person ages. Sometimes called degenerative disc disease or osteoarthritis, spondylosis also encompasses other conditions that cause deterioration in the spine, such as stenosis. Disc degeneration and herniation, bone spurs and stiff ligaments may all contribute to spondylosis.
A person with spondylosis may be asymptomatic, but pain and stiffness may develop as time passes. These symptoms may be worse in the morning and improve as the day progresses. The pain occurs in the area in which the degeneration has occurred, so a person with spondylosis may have pain and stiffness in the neck or anywhere in the back. If a nerve becomes pinched or irritated, they may notice numbness, tingling, weakness or shooting pain in their legs.
Doctors diagnose spondylosis based on a physical exam, the person’s symptoms and imaging tests, such as X-rays, MRIs and CT scans.
How Common Is Spondylosis?
Spinal changes occur as people age and often begin during the third decade of life. Approximately 90% of people have cervical spondylosis by the time they’re 60 years old.
People who smoke, have previous neck or back injuries or have family members with spondylosis are more likely to develop the condition. Those whose jobs involve heavy lifting, neck strain or exposure to vibration are at greater risk of developing spondylosis.
Common Treatments for Spondylosis
Engaging in regular exercise, applying heat and ice and taking over-the-counter pain medications may alleviate discomfort. Doctors may prescribe pain medications, muscle relaxants, corticosteroids and antidepressants as well, and they may suggest physical therapy, acupuncture or spinal manipulation.
Spinal injections may also help relieve pain. In extreme cases, vertebrae fusion or surgical removal of a herniated disk, bone spur or vertebra may be necessary.
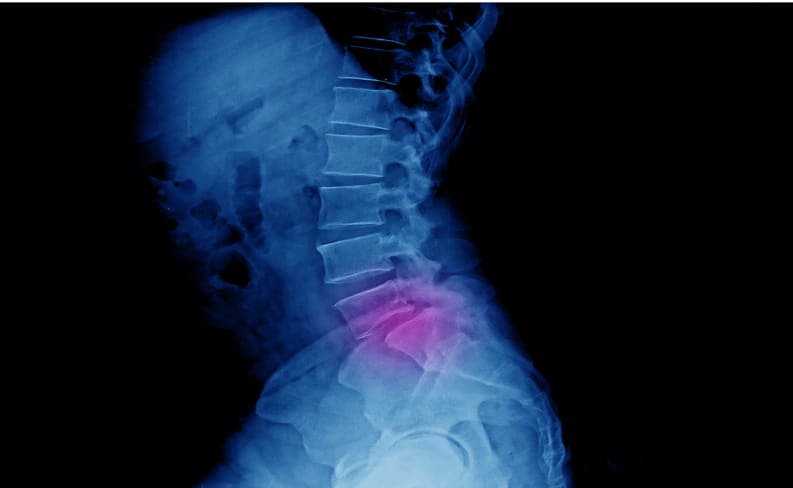
Spondylolisthesis

What Is Spondylolisthesis?
Spondylolisthesis occurs when a vertebra slips out of position onto the vertebra below it. While the lower back is typically affected, any part of the back may be impacted. Spondylolisthesis can occur as the result of an injury (isthmic spondylolisthesis), or it may develop as the spine degenerates with age (degenerative spondylolisthesis).
Sometimes, people with spondylolisthesis have no symptoms, but others may experience tenderness in the region of the displaced vertebra, lower back pain, stiffness and muscle tightness. Other symptoms may include leg weakness as well as pain or numbness in the buttocks and thighs.
How Common Is Spondylolisthesis?
Approximately 5 to 7% of the population may have spondylolisthesis resulting from an injury. Young people who engage in sports that involve repetitive overstretching, such as gymnastics and football, are more likely to develop isthmic spondylolisthesis. Birth defects, bone abnormalities and spinal trauma may also cause the condition.
Degenerative spondylolisthesis typically affects people over 50, and women are more likely to be impacted than men. Wear and tear on the bones and cartilage and the development of arthritis are factors that play roles in the development of degenerative spondylolisthesis.
Common Treatments for Spondylolisthesis
Symptoms of spondylolisthesis often respond to conservative treatments, such as resting, taking nonsteroidal anti-inflammatory medications and receiving corticosteroid injections. Using a brace may offer support while healing takes place. Physical therapy may be helpful in stretching and strengthening muscles and improving flexibility.
A surgical procedure is available to fuse shifted bones. This intervention is reserved for those with severe pain that doesn’t respond to treatment and cases where leg weakness or lack of bowel or bladder control are present. It’s also used to correct a severe bone shift.
Degenerative Disc Disease
What Is Degenerative Disc Disease?
Degenerative disc disease occurs when the tough outer casing of the discs between your vertebrae cracks or dries out. It can irritate nerves in the disc wall or stop the disc from absorbing shocks as effectively.
Not everyone with degenerative disc disease has symptoms, but it can cause neck or back pain, which may radiate down the legs or buttocks. It can also reduce flexibility in your spine and make it harder to twist or bend your back.
Sometimes, degenerative disc disease causes the disc wall to herniate, allowing the disc’s soft center to bulge out and press on nearby nerves. This can cause severe pain and changes in sensation in your hands and feet, such as pins and needles.
How Common Is Degenerative Disc Disease?
Degenerative disc disease is common, and your risk of developing it increases as you get older. The chance of having degenerative disc disease roughly correlates with age. Therefore, around 40% of 40-year-olds have degenerative disc disease, increasing to 80% of people in their eighties.
Common Treatments for Degenerative Disc Disease
A common treatment for degenerative disc disease is spinal decompression therapy. During treatment, a device is used to gently stretch the spinal column to reduce pressure on the discs. This encourages herniated discs to move back into the correct position and reduces pressure on the spinal nerves to relieve stiffness and pain.
If degenerative disc disease is causing pain, over-the-counter or prescription painkillers may help reduce discomfort. Many people find that applying heat or ice packs to the affected area provides some relief.
If more conservative treatment methods don’t work, surgery may be required to remove the fault disc (discectomy) or join the surrounding vertebrae together (spinal fusion).
Facet Syndrome
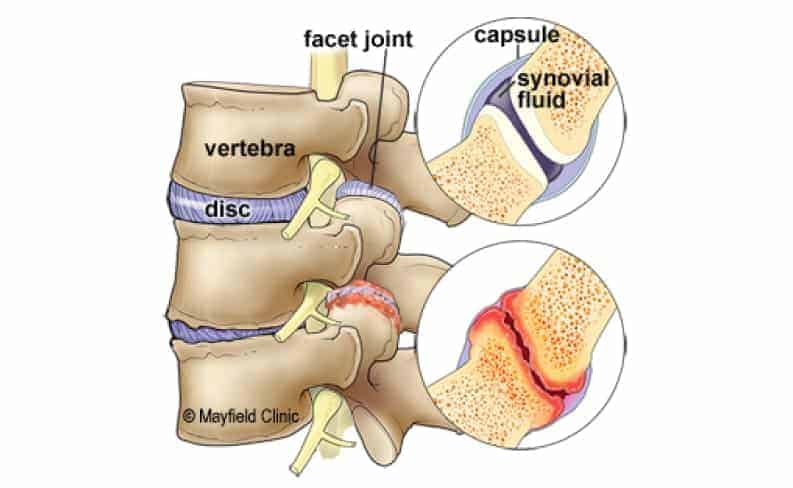
What Is Facet Syndrome?
Facet joints in the spine provide stability and support when the spine is twisted. In someone with facet syndrome, the joints become worn or inflamed. Small nerve fibers in the joint can cause pain due to swelling or joints rubbing against each other.
The location of facet syndrome pain can be difficult to predict and depends on which facet joints are affected. Pain mostly occurs in the lower back and can spread to the buttocks and legs. However, facet syndrome can also cause pain in the upper back, shoulders and neck. The syndrome can also lead to headaches.
How Common Is Facet Syndrome?
Up to 80% of people will experience a back problem at some point in their lives, and facet syndrome is a common source of back pain. Problems with lumbar facet joints are the cause of up to 45% of lower back pain. Normal wear and degeneration over time cause most cases of facet syndrome, but an injury to the spine can also lead to problems with facet joints. People who have osteoarthritis, are obese or smoke may be at increased risk for facet syndrome.
Common Treatments for Facet Syndrome
Anti-inflammatory medications and physical therapy are common recommendations for less severe cases. Physical therapy can help build muscles that stabilize the spine, providing pain relief and preventing further damage. Acupuncture and chiropractic therapy can also help relieve back and neck pain.
Facet injections deliver medication directly to the joint and can be an effective way to relieve pain and swelling. However, a person may need multiple injections for lasting effects. For severe cases, surgery to remove sensation from the painful nerve fibers may offer long-term relief.
Headaches

Why Does Back Pain Cause Headaches?
Headaches can occur for numerous reasons, including stress, emotional changes, dehydration, eye strain, excessive medication use or sinus pressure. One common cause of headaches is actually pain or strain in the back or neck.
Back pain and headache can occur together for reasons that include injury to the spine or back, poor posture that puts strain on muscles, and infections. Pre-existing conditions — including arthritis, IBS and fibromyalgia — can also cause back pain and headache, and these symptoms might also be prevalent during pregnancy or times when a woman is dealing with symptoms of premenstrual syndrome.
How Common Are Headaches With Back Pain?
Headaches are an extremely common symptom for adults. Three out of every four American adults report having a headache in the past 12 months.
Studies have indicated a correlation between back pain and headache. It’s fairly common to experience headache as a side effect of a back problem, but individuals might also experience headache and back pain together as symptoms of other underlying conditions.
Common Treatments of Headaches Associated With Back Pain
Common treatments for headaches include resting and taking over-the-counter pain relievers such as aspirin, acetaminophen and NSAIDs. Depending on the type of headaches, changes in diet and lifestyle may also help reduce the issue. If headache and back pain are both present, treating any underlying problems can be important.
Treatment for headaches seemingly caused by back pain requires treating the back pain itself. Chiropractic manipulation, acupuncture, trigger point injections and physical therapy are some common treatment options.
TMJ Disorder

What Is TMJ Disorder?
The temporomandibular joint connects the jaw to the side of the head, making it possible to chew, talk and perform other mouth movements. TMJ stands for temporomandibular joint disorder, a condition that causes pain in the jaw and difficulty opening or closing the mouth. Additional symptoms include stiffening of the jaw muscles, neck pain, a clicking sound in the jaw, pain in the face and reduced range of motion in the jaw.
Although TMJ disorder mainly affects the jaw, some people with this condition also have back pain. TMJ dysfunction can cause back pain by pushing the jaw out of alignment, which puts extra stress on the neck muscles. The extra stress can change the way the neck and back muscles work together, resulting in ongoing back pain. Although TMJ disorder can develop in anyone, certain people have an increased risk of developing it. The risk is higher in people with jaw injuries, connective tissue diseases and arthritis, as well as people who tend to clench or grind their teeth.
How Common Is TMJ Disorder?
The National Institute of Dental and Craniofacial Research estimates that more than 10 million Americans have some type of TMJ disorder.
Common Treatments for TMJ Disorder
Treating TMJ disorder can help relieve back pain and other symptoms associated with the condition. Eating soft foods, taking over-the-counter pain relievers, applying ice or heat, wearing a night guard and avoiding certain jaw movements can all help relieve the symptoms of TMJ disorder without surgery.
If a conservative approach isn’t effective, a doctor or dentist may recommend trigger-point injections, ultrasound, radio wave therapy, Botox injections or transcutaneous electrical nerve stimulation. Chiropractic manipulation of the jaw and muscles that connect the jaw to the spine have also shown to provide relief from TMJ.
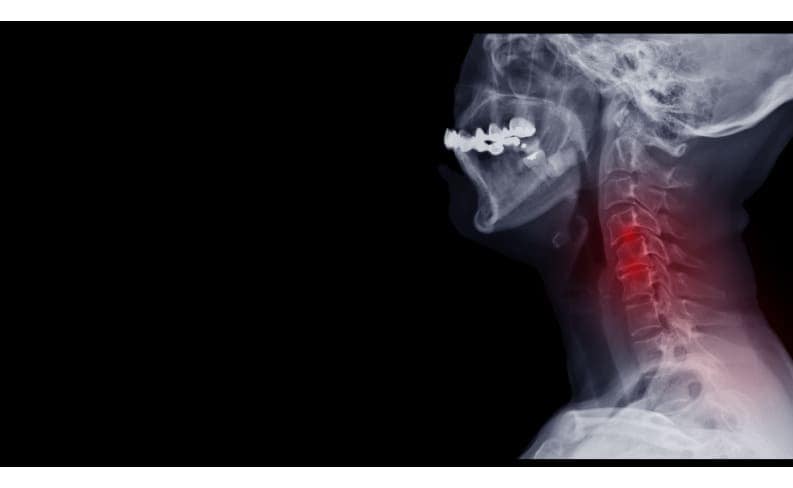
Radiculopathy
What Is Radiculopathy?
Radiculopathy is a term that refers to a pinched nerve. Although pinched nerves may occur in the hands, elbows or wrists, they most often develop in the spine where they may cause pain, numbness, weakness and tingling in the back, arms, hands, legs or neck. The symptoms vary depending on the affected nerve’s location in the spine. Sometimes, no symptoms are present, or they only flare up periodically.
How Common Is Radiculopathy?
Approximately 85 of every 100,000 adults in the United States experience a pinched nerve each year. Radiculopathy can affect people of any age, but it’s more common in those over age 50 because they’re more prone to arthritis and spinal degeneration that narrows the available space for nerve roots.
Radiculopathy most often occurs in the lower back, where it may be called sciatica. This may cause pain that radiates from the lower back down the leg to the foot. Cervical radiculopathy develops when a nerve root in the neck is pinched, and symptoms may present in the arms and hands. The least common location for radiculopathy is the chest, or thoracic area. Symptoms of thoracic radiculopathy may include pain and numbness that wraps around the chest.
Common Treatments for Radiculopathy
Radiculopathy symptoms often diminish with time and rest, but applying ice or heat to the affected area and taking over-the-counter pain medications may help ease discomfort. A doctor may also administer steroid injections to alleviate pain and inflammation. Depending on the body part involved, splints or cervical collars may help limit motion while healing takes place.
Physical therapy, spinal manipulation and exercises may be helpful, with exercises and stretches that help alleviate pressure on the impacted nerves. In some cases, surgical removal of discs or bone is an option to help relieve pressure on the nerve.
Ankylosing Spondylitis
What Is Ankylosing Spondylitis?
A form of arthritis, ankylosing spondylitis (AS) causes long-term inflammation of the spine. The inflammation typically first appears in the sacroiliac joints between the base of the spine and the pelvis. It then can spread to joints between the vertebrae. As time passes, new bone may form, fusing some of the vertebrae together.
Early symptoms may include lower back pain and stiffness, which may feel worse in the morning or following periods of inactivity. Neck pain and fatigue may also be present. Symptoms may become more severe as time goes on. Eye inflammation and heart problems may also develop, and if the rib cage is affected, breathing may become more difficult.
How Common Is Ankylosing Spondylitis?
AS belongs to the group of diseases known as spondyloarthropathies, which affect between three and 13 out of every 1,000 Americans. Since most people with AS have a mutation of the HLA-B gene, AS may be hereditary. However, not everyone with that gene mutation develops AS.
Symptoms often arise during late adolescence or early adulthood and typically affect males more frequently than females. People with Crohn’s disease, psoriasis and ulcerative colitis may also be more prone to developing AS.
Common Treatments for Ankylosing Spondylitis
Lifestyle adjustments — such as avoiding fried or processed foods and foods with high fat or sugar contents, refraining from smoking, limiting alcohol intake and maintaining a healthy weight — may help reduce pain and inflammation. Regular exercise may help slow the progression of AS while improving strength and flexibility and reducing pain.
Oral nonsteroidal anti-inflammatory drugs, disease-modifying anti-rheumatic drugs (DMARDs) and injected corticosteroids may mitigate pain and inflammation. Doctors may suggest surgical intervention If severe pain or joint damage occurs.
Scoliosis

What Is Scoliosis?
A normal spine has natural curves that help the body maintain a normal position and distribute shock evenly while walking, running and performing other movements. In people with scoliosis, the spine curves sideways, causing back pain and other symptoms. These symptoms include uneven shoulders, leaning to one side, misalignment of the rib cages and hairy patches or dimples over the curved part of the spine. Although pain is one of the most common symptoms of scoliosis, the condition may also cause reduced lung function due to changes in the size and shape of the chest cavity and associated structures.
Some cases of scoliosis are caused by spine abnormalities that appear during fetal development. This is known as congenital scoliosis. Scoliosis can also be caused by cerebral palsy, spina bifida, muscular dystrophy and other neuromuscular diseases. This is known as neuromuscular scoliosis. A diagnosis of scoliosis is usually made when an X-ray reveals that the spine has a sideways curvature of 10 degrees or more.
How Common Is Scoliosis?
In the United States, about three million new cases of scoliosis are diagnosed each year.
Common Treatments for Scoliosis
If the abnormal curve is less than 20 degrees, doctors may recommend repeat X-rays to determine if the curve is getting worse or staying the same. Bracing is an option when the curve is progressive or when the initial curve is between 20 and 40 degrees. Wearing a brace may prevent the curve from becoming severe enough to require surgery. Some people need a surgical procedure called spinal fusion to lessen the curve and relieve scoliosis-related pain. During a spinal fusion, the surgeon fuses several vertebrae together to form a single bone. A rod is typically left in place to support the spine as it fuses.
Kyphosis

What Is Kyphosis?
Kyphosis is a condition where the spine curves forward more than 50 degrees, producing a noticeably rounded appearance. It can also cause pain and hamstring tension. There are several types of kyphosis.
Individuals with postural kyphosis have anatomically normal vertebrae, and their condition is often caused by incorrect posture. Scheuermann’s kyphosis occurs when the vertebrae have an abnormal, wedge-like shape. Occasionally, people are born with abnormally shaped vertebrae, causing a curved spine. This is known as congenital kyphosis. Scheuermann’s and congenital kyphosis tend to get worse as the affected individual grows.
Kyphosis is associated with several other conditions. People with spina bifida, osteogenesis imperfecta (brittle bone disease) and certain metabolic and neuromuscular problems are more likely to develop kyphosis.
How Common Is Kyphosis?
Postural kyphosis is relatively common during adolescence, especially among individuals who slouch. Older adults are also at a higher risk of kyphosis related to brittle bone disease, and the condition is present between 20 and 40% of people over 60. Females have a higher risk of developing postural and age-related kyphosis.
Scheuermann’s kyphosis affects between 0.4% and 8% of the population and usually becomes apparent in adolescence. Males have a 50% higher chance of developing Scheuermann’s kyphosis compared to females.
Common Treatments for Kyphosis
Postural kyphosis rarely causes adverse health effects, but physical therapy can help strengthen the core muscles and improve posture to reduce abnormal curvature and pain. Some affected individuals choose to wear a brace to make the spine’s curvature less noticeable, and braces can also successfully correct kyphosis if the person is still growing.
In cases where the condition causes severe pain or curvature or results from a congenital problem, doctors may recommend spinal fusion surgery. This treatment involves connecting two or more vertebrae using metal screws to create a normal curvature.
Sacroiliitis

What Is Sacroiliitis?
A common cause of pain in the lower back, buttocks or thighs, sacroiliitis is an inflammation of one or both sacrum joints, which are located at the junction of the lower back and pelvis. The pain may be dull and achy or sharp and stabbing, and it may extend to the legs, groin and feet. Standing or sitting for long periods of time, climbing stairs, rotating the hips, running and taking large strides may cause the pain to worsen.
How Common Is Sacroiliitis?
It’s difficult to say how many people have sacroiliitis because its symptoms are similar to those related to other back problems. Between 10% and 25% of people with low back pain may have sacroiliitis.
Common causes of sacroiliitis include trauma, infection and some types of arthritis. Loosening and stretching of the sacroiliac joints during pregnancy may also lead to sacroiliitis, especially when factoring in the added stress on these joints due to the extra weight that accompanies pregnancy.
Common Treatments for Sacroiliitis
Physical therapy is typically helpful in alleviating the pain from sacroiliitis, incorporating range-of-motion and stretching exercises to enhance flexibility and strengthen muscles. Pain relievers and muscle relaxants may bring relief, as can corticosteroid injections.
Radiofrequency ablation uses radio waves to heat and destroy a small area of nerve tissue to prevent further transmission of pain signals. Alternatively, implanting an electrical stimulator in the sacrum may alleviate pain. In rare cases, doctors may recommend joint fusion to mitigate the pain.
Coccydynia

What Is Coccydynia?
Coccydynia refers to pain in the coccyx or tailbone, which is the bone at the end of the spine, and it may manifest as a dull ache or a stabbing pain. Degenerative changes, trauma from a fall or difficult childbirth and sitting for long periods on a hard surface may cause coccydynia. Other possible causes of coccydynia include infections, abscesses and tumors.
Tailbone pain may become more severe during sitting, prolonged standing, defecating and engaging in sexual intercourse. In women, the pain may also cause increased discomfort during menstruation.
How Common Is Coccydynia?
Coccydynia is a common condition that occurs more frequently in adults than in children. Women are five times more likely than men to experience tailbone pain, and those who are obese are more prone to coccydynia than people who keep their weight within normal limits. People who experience rapid weight loss are also more likely to develop tailbone pain.
Common Treatments for Coccydynia
Coccydynia normally resolves without treatment within a few weeks or months. Taking over-the-counter pain medications, applying heat or ice to the painful region, sitting on a doughnut-shaped cushion and leaning forward when sitting are some measures that may help alleviate discomfort while healing takes place. Wearing loose clothing may be beneficial as well, and taking stool softeners may help stool pass with less discomfort.
Acupuncture, massage therapy and exercises to stretch and strengthen muscles and improve posture may provide relief from tailbone pain. A doctor may use numbing agents and steroids to block the nerve supply in the affected area. In very rare cases, a doctor may perform a surgical procedure to remove all or part of the coccyx to help alleviate the pain.
Thoracic Outlet Syndrome

What Is Thoracic Outlet Syndrome?
Nerves connecting the upper spine to the arms pass through an opening between the collarbone and ribs called the thoracic outlet. Veins and arteries responsible for blood flow in the arms and hands also pass through this space.
When these nerves and blood vessels become pinched or compressed, they cause thoracic outlet syndrome (TOS). Neurogenic TOS primarily affects the nerves between the arms and the spinal cord. Venous and arterial TOS cause the compression of the blood vessels. TOS that compresses a blood vessel is also sometimes called vascular TOS.
Thoracic outlet syndrome can have a variety of causes, including:
- Repetitive motions
- Traumatic injuries, such as those caused by car accidents and falls
- Poor posture
- Anatomical reasons, such as the presence of an extra rib
Symptoms can include pain in the upper back, shoulders and arms. People with TOS may also experience tingling, numbness and weakness in their arms or hands. If left untreated, the syndrome can cause permanent nerve damage.
How Common Is Thoracic Outlet Syndrome?
People between the ages of 20 and 40 are most likely to be affected by TOS. Women are significantly more likely than men to experience TOS and may first experience symptoms during pregnancy. Neurogenic TOS makes up around 95% of cases of TOS.
Common Treatments for Thoracic Outlet Syndrome
Physical therapy, chiropractic services and anti-inflammatory medications are common early treatments for TOS. These treatments often provide effective pain relief and avoid additional nerve damage.
A patient with neurogenic TOS may need surgery if more conservative therapies don’t work. TOS involving the compression of blood vessels is more likely to require surgery.
Foraminal Stenosis
What Is Foraminal Stenosis?
The spine has multiple openings called foramen, which typically have enough room for the nerves extending from the spinal cord to connect to other parts of the body. In people with foraminal stenosis, at least one of these openings becomes narrower, causing weakness, numbness and unusual sensations in the arms and legs. Foraminal stenosis is classified as a type of spinal stenosis.
How Common Is Foraminal Stenosis?
As many as 500,000 U.S. residents have spinal stenosis. Although foraminal stenosis can occur anywhere in the spine, it’s most common in the lumbar area. Degenerative disc disease and spondylosis tend to occur in the lumbar area, further increasing the risk of foraminal stenosis in this part of the spine.
Common Treatments for Foraminal Stenosis
For mild foraminal stenosis symptoms, a doctor may recommend aspirin or ibuprofen to relieve pain. Corticosteroid shots are also an option, as they reduce inflammation in the affected nerve root. If foraminal stenosis results in reduced range of motion, activity restriction may be necessary. Depending on the severity of the symptoms, people with foraminal stenosis may have to adjust their exercise routines or ask for job modifications to give their bodies time to recover. Wearing a brace is another nonsurgical option for treating foraminal stenosis.
If the symptoms don’t respond to nonsurgical treatments, a surgeon may recommend a foraminotomy. During this procedure, the surgeon enlarges the space around the affected foramen. This reduces the amount of pressure on the surrounding nerves, relieving pain, weakness, numbness and other symptoms. A person who has a foraminotomy should expect to stay in the hospital for at least a day or two. If the foraminotomy was performed on the cervical spine, the surgeon may also recommend wearing a neck brace and avoiding certain movements.
Get Help With Back Pain Today
Whether you’re dealing with a pain in your back or are in recovery after an injury or treatment, we can help. Contact us today to learn about your options or to schedule an appointment.
